Single-Path Medical Coding Services
Unify facility and pro-fee coding in one expert workflow. Single-path medical coding is the assignment of both the outpatient facility and the professional (pro-fee) codes for the same encounter in a single session by one highly skilled coder. The result: fewer discrepancies, faster cash, and tighter compliance for high-volume outpatient service lines like Emergency Department (ED), hospital outpatient clinics, radiology/imaging, observation, and ambulatory surgery.
Background
Traditional workflows split professional and facility coding across different teams, creating duplicate work, inconsistent code sets, reconciliation headaches, and preventable denials. Single-path coding eliminates that friction: one coder reviews the chart once, applies the correct professional and facility rules, and reconciles both claim types before submission.
Why Organizations Move to Single-Path
- Cleaner, consistent claims: One coder aligns professional and facility code sets—reducing mismatches that trigger denials.
- Speed & efficiency: One documentation review, one coding session—shorter coding lag and faster first-pass payments.
- Lower cost-to-code: Eliminates duplicate touches and inter-team back-and-forth.
- Better governance: Standardized edits, queries, initial and ongoing QA, and reporting across both sides of the claim.
- Documentation uplift: Targeted feedback closes gaps that affect both claims.
- Scales well: Ideal for ED, imaging, clinics, observation, and same-day surgery volumes.
The Coding Network Difference
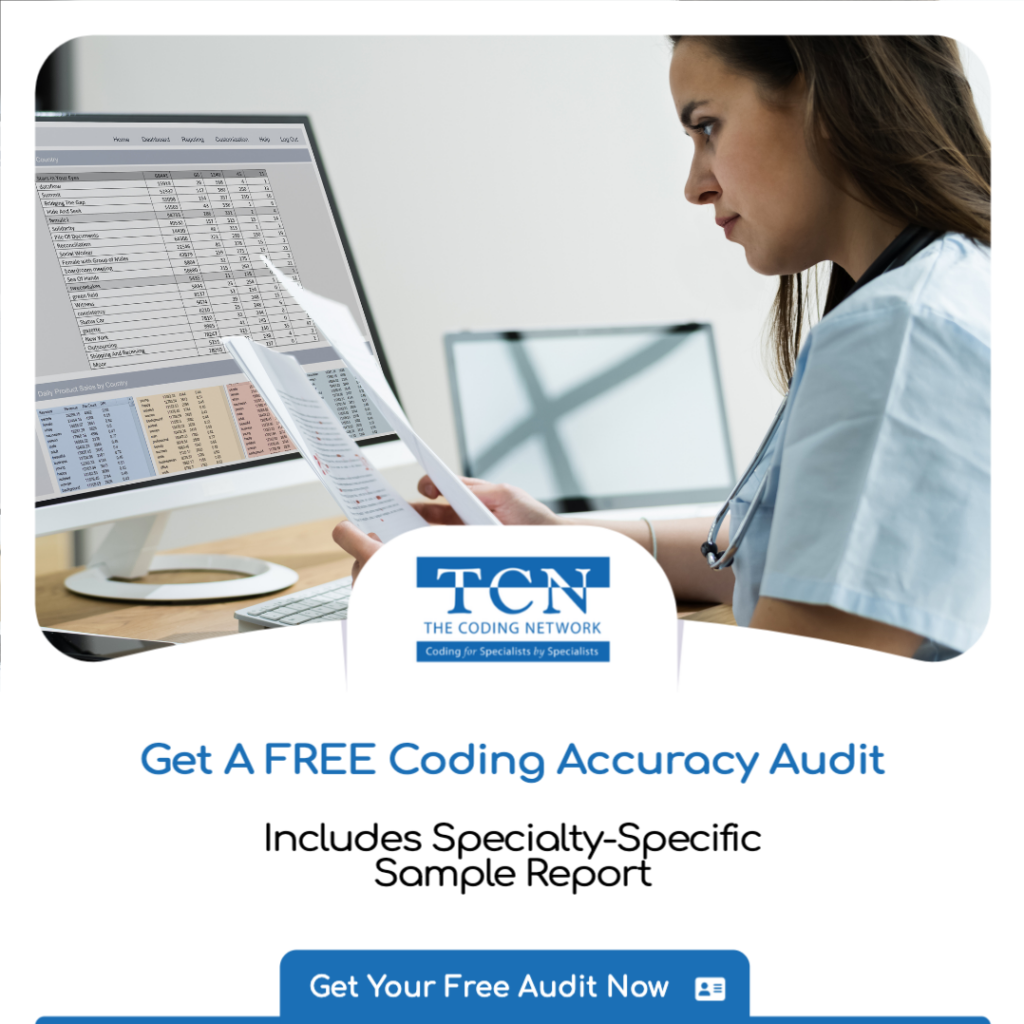
- U.S.-based, specialty-specific coders and auditors: 900+ experts across the full spectrum of medical and surgical specialties.
- Quality bar: Specialty proficiency testing and ongoing random QA with a ≥90% accuracy requirement.
- Reliable turnaround: Consistently sent volumes coded within 2–3 business days.
- No minimums: Send all or part of your daily volume; ideal for pilots, overflow, or staffing gaps.
- Flexible engagement: Per-case pricing, temporary or ongoing coverage, rapid onboarding.
- Beyond coding: Documentation training, compliance audits, helpline support, and denial analysis.
How Our Single-Path Service Works
- Intake & profile setup
We configure your coding profile (payers, edits, local rules) and connect to your EHR/encoder workflow for secure remote coding. - Unified encounter review
A TCN coder reviews the chart once and assigns both outpatient facility and professional codes in one workflow. The number of coders required for managing a coding queue depends on the volume of cases needed to be coded and the number of specialties involved. - Edits, queries, reconciliation
We clear edits, issue necessary provider queries, and align technical/professional components before submission. - Quality assurance
Ongoing random QA against our accuracy benchmark, with feedback to providers and revenue-cycle teams. - Reporting & continuous improvement
Documentation gap insights, and targeted education to drive measurable gains.
Service Scope
Settings
- Emergency Department (ED)
- Hospital outpatient clinics
- Diagnostic & interventional radiology / imaging
- Observation Unit
- Same-day outpatient / Ambulatory surgery centers
- Interventional Labs
- Pathology
Coding Sets & Rules
- ICD-10-CM, CPT®, HCPCS Level II
- OPPS/APC logic for facility; pro-fee guidelines for clinicians
- Local payer policies and edits per your profile
Measurable Outcomes
- Reduced denial rates from pro-fee/facility mismatches
- Shorter DNFB and coding lag
- Improved first-pass yield and clean-claim rates
- Actionable provider documentation improvements
Getting Started
Pilot single-path coding in one department (ED or radiology is common) or expand across multiple outpatient service lines. We’ll tailor a rollout plan, success metrics, and governance to your environment—without minimums and with rapid, secure onboarding. Request a proposal to unify your outpatient coding.
Single-Path Coding FAQ
What is single-path medical coding?
A unified workflow where a coder reviews the chart once and assigns both the outpatient facility and professional codes for the same encounter. It’s designed to reduce discrepancies, speed up billing, and simplify governance.
Where does single-path make the biggest impact?
ED, hospital outpatient clinics, radiology/imaging, observation, and same-day surgery—settings where technical and professional services occur together and are billed separately today.
Is this only for outpatient?
Single-path coding is primarily outpatient driven. For inpatient, facility and pro-fee workflows usually remain distinct due to different rules and documentation patterns, but our QA and reconciliation practices can still align outputs across teams.
What turnaround time can we expect?
For consistently sent volumes, our standard turnaround is 2–3 business days (can be 2 to 3 calendar days).
Do you require volume minimums or long-term commitments?
No. There are no per-case minimums or duration of utilization. We support pilots, overflow,backlogs, and ongoing coverage, so you can reduce overtime expenditures.
Are your coders U.S.-based?
Yes. All Coding Network coders and auditors live and work in the United States.
How do you ensure accuracy and compliance?
Specialty-specific coders must undergo rigorous proficiency testing. We perform ongoing random QA reviews with a ≥90% accuracy requirement and provide documentation feedback and denial analytics to drive continuous improvement.
What technology do you use?
We securely log into your EHR/encoder (or set up a secure file workflow) and operate within your coding profile and payer policies. We align edits and queries across both professional and facility claims in one standardized process. Therefore we are technologically agnostic and can operate within any system of combination of systems.
How do we start a pilot?
Choose one department (ED or radiology is common). We’ll define scope, volumes, SLAs, and success metrics; configure your coding profile; and begin coding within the agreed timeline—then expand based on results.
The TCN Advantage
At TCN, we stand apart with decades of industry experience and a proven track record of excellence. Combining deep clinical knowledge with advanced technology, rigorous quality assurance, and a commitment to personalized service makes this solution optimal for the integration and adoption of AI based coding solutions. We deliver custom workflows that are not only accurate and compliant but also seamlessly integrated into your organization’s revenue cycle system —ensuring you achieve maximum value from your AI investment.
By partnering with TCN for AI Medical Coding Validation and Audits & Compliance Reviews, you’re not only leveraging advanced technology—you’re ensuring that technology consistently delivers on its promise of efficiency, accuracy, and compliance through the trusted expertise that has defined TCN for years.
Contact us today to learn how we can help you protect your revenue and elevate your coding operations in the age of AI.
—
Latest Blog Posts:
Why Human Oversight in AI Medical Coding Remains Essential in 2025
The emergence of AI in medical coding is invariably impacting healthcare and traditional workflows and resource allocation. Yet, as AI platforms tout accuracy rates exceeding 90%, a critical question persists: Can autonomous coding stand alone? [...]
AI Medical Coding Is Fast—Until Compliance Slows You Down
Why Human Validation Is Now Mission‑Critical (and How to Add It Overnight) Artificial‑intelligence engines from Aidéo, Fathom, Nym, 3M, and others are transforming medical coding speed. Yet payers haven’t lowered the bar— they’ve raised it. Humana, [...]
How to Dodge the Holiday Coding Backlog – Without Adding Full‑Time Staff
Summer vacations fill the calendar, and Labor Day marks the starting line of a four‑month holiday sprint. For revenue‑cycle leaders, that means one thing: charts start stacking up on Friday, coders walk in Monday to a [...]
Need Professional Medical Coding Assistance: Why Using Your Doctors To Code Is Not Free
In today’s fast-paced healthcare environment, efficiency and accuracy are non-negotiable. Every medical practice, hospital, and healthcare system strives to optimize revenue, ensure compliance, and deliver exceptional patient care. One area that often flies under the [...]